The pancreas is a vital organ involved in digestion and blood sugar regulation, but what happens if it fails or needs to be removed? Many wonder, can you live without a pancreas? The answer is yes—with significant medical support and lifestyle adjustments, people can survive after pancreas removal. This article will explore the functions of the pancreas, the implications of living without it, and how medical advancements enable survival and quality of life.
What Is the Pancreas and Why Is It Important?
The pancreas is a gland located behind the stomach that performs two critical functions:
Exocrine Function: Digestive Enzymes Production
It produces enzymes that help break down fats, proteins, and carbohydrates in the small intestine.
Endocrine Function: Hormone Production
It releases important hormones, primarily insulin and glucagon, which regulate blood sugar levels.
Without these functions, the body faces challenges in digestion and glucose control.
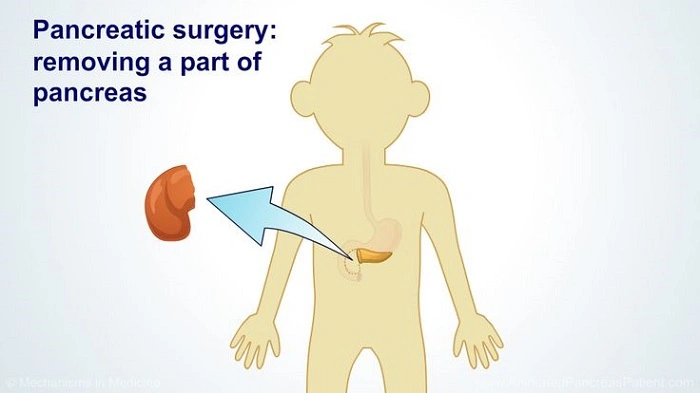
Causes for Pancreas Removal (Pancreatectomy)
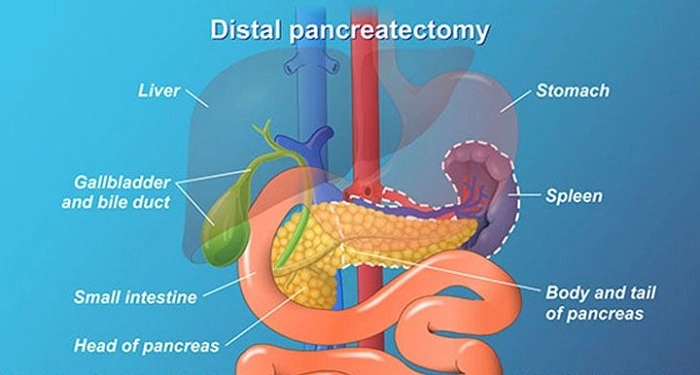
Sometimes, the pancreas needs to be surgically removed due to:
- Pancreatic cancer
- Chronic pancreatitis causing severe damage
- Trauma or injury to the pancreas
- Benign tumors or cysts affecting pancreatic function
Depending on the extent, surgeons may perform a total or partial pancreatectomy.
What Happens When the Pancreas Is Removed?
Removal of the pancreas causes the loss of both its digestive enzyme production and insulin secretion, leading to two major medical conditions:
1. Exocrine Pancreatic Insufficiency (EPI)
Without digestive enzymes, the body cannot properly digest food, especially fats, leading to malnutrition, weight loss, and gastrointestinal symptoms.
2. Surgical or “Pancreatogenic” Diabetes
Since insulin production ceases, patients develop diabetes that requires lifelong insulin therapy to control blood sugar levels.
Can You Live Without a Pancreas?
Yes, but living without a pancreas requires:
- Lifelong enzyme replacement therapy to aid digestion
- Daily insulin injections or insulin pump therapy to manage diabetes
- Regular monitoring of blood sugar and nutritional status
- Close medical supervision from endocrinologists and gastroenterologists
With these treatments, many patients live productive lives post-pancreatectomy.
Managing Life After Pancreas Removal
Enzyme Replacement Therapy
Taking pancreatic enzyme supplements with meals helps improve digestion and nutrient absorption, reducing symptoms like diarrhea and bloating.
Insulin Therapy
Since natural insulin is no longer produced, patients must manage blood glucose levels with external insulin through injections or pumps. Continuous glucose monitoring is often recommended.
Dietary Adjustments
Patients are advised to:
- Eat smaller, frequent meals
- Focus on easily digestible foods
- Limit high-fat foods
- Maintain proper hydration
Regular Medical Follow-Up
Frequent check-ups help manage complications and adjust treatments as needed.
Potential Complications Without Proper Management
Without adequate enzyme or insulin replacement, patients can experience:
- Severe malnutrition and vitamin deficiencies
- Dangerous blood sugar fluctuations, including hypoglycemia and hyperglycemia
- Weight loss and weakness
- Increased risk of infections
Therefore, compliance with medical treatment is critical.
Advances in Treatment and Research
Ongoing research aims to improve quality of life for people living without a pancreas, including:
- Improved pancreatic enzyme formulations
- Advanced insulin delivery systems
- Islet cell transplantation (experimental)
- Artificial pancreas development for automated glucose control
These innovations hold promise for reducing the burden of pancreas loss in the future.
Frequently Asked Questions About Living Without a Pancreas
Can I survive if my entire pancreas is removed?
Yes, but you will need lifelong enzyme replacement and insulin therapy.
How is diabetes managed after pancreas removal?
Through regular insulin injections or an insulin pump combined with frequent blood sugar monitoring.
Are there alternatives to complete pancreas removal?
Sometimes partial removal or other treatments are possible depending on the condition.
What dietary changes are needed post-pancreatectomy?
A low-fat, nutrient-rich diet with smaller meals is recommended, along with enzyme supplements.
Is pancreas transplantation an option?
Pancreas transplant is rare and usually reserved for select diabetic patients but is not common after total pancreas removal for cancer.
Living without a pancreas is medically challenging but entirely possible with proper care. Pancreas removal leads to digestive and metabolic changes requiring lifelong management of enzyme deficiency and insulin-dependent diabetes. Thanks to modern medicine and personalized treatment plans, many individuals lead fulfilling lives post-pancreatectomy. If you or a loved one faces pancreas removal, understanding these treatments and maintaining close medical follow-up are essential for health and quality of life.